- Cancer Immunotherapy - (https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/immunotherapy.html)
- Immunotherapy: Using the Immune System to Treat Cancer - (https://www.cancer.gov/research/areas/treatment/immunotherapy-using-immune-system)
- What is immunotherapy? - (http://sitc.sitcancer.org/userfiles/file/cancerimmunotherapyfaqs.pdf)
- The Next Great Advance in Cancer Treatment - (http://www.cancerresearch.org/cancer-immunotherapy)
What is Cancer Immunotherapy?
Cancer immunotherapy is a new advancement in cancer treatment that uses certain components of a person’s immune system to fight against cancer cells.
It is a kind of biological therapy because it uses substances derived from living organisms.
Immunotherapy in a broader sense is a type of treatment that works by
- Enhancing or stimulating the immune system - Eg. Activation immunotherapies that destroy cancer cells.
- Inhibiting or suppressing the immune system - Eg. Suppression immunotherapies that suppress the immune system to treat allergies and after organ donations.
Facts on Cancer:
- Worldwide, 14.1 million people were diagnosed with cancer in the year 2012
- Nearly 8.2 million people died due to cancer in 2012
- Cancer deaths among women have been predicted to increase twofold by the year 2030
How does Immunotherapy Work against Cancer?
The immune system contains certain cells and substances that help us fight against infections. They know which substances are normally present within the body and which are foreign. When they see foreign objects like specific proteins (antigens) on germs, they produce counter-attack proteins called antibodies to fight them. The same goes for antigens on cancer cells; the immune cells also produce an immune response against the cancer cells too but they can only fight cancer cells up to a certain point.
This is because, sometimes,
- The cancer cells do not look very different from normal cells
- The immune system recognizes the cells but does not produce a strong enough response
- The cancer cells themselves have the ability to keep the immune system at bay
The cancer cells that remain, overcome the immune system and multiply forming detectable tumors. Now the cancer is too hard to fight and the immune system needs assistance. That’s where immunotherapy comes in. Immunotherapy brings the immune system to a higher level to fight cancer again in order to achieve a complete, long-lasting cure for patients.
The benefits of immunotherapy are
- Specificity - Targets only cancer cells; does not affect other cells
- Good reach - Works systematically killing cancer cells all over the body
- Memory - Creates a memory so it can also protect against cancer in the future
- Broad range - Can be used for all kinds of cancers
What are some of the Components of the Immune System and their Functions?
- Regulatory T cells: These cells tell the immune system when and where to stop attacking.
- B cells: These cells churn out antibodies by the dozen to attack. Antibodies are the ammunition that the body uses to bind to certain proteins on cancer cells debilitating them and marking them as targets for other immune cells
- CD8+ Killer T cells: These set out and vigorously kill the cancer cells.
- CD4+ Helper T cells: These coordinate the responses of the B cells and the CD8+ Killer T cells.
- Cytokines: Cytokines help the different kinds of immune cells communicate with each other to bring about the right attack.
- Dendritic cells: These process antigen material and present it on the cell surface to the T cells. They are also called antigen-presenting cells or APCs.
What are the Types of Immunotherapy in Cancer Treatment?
There are four types of immunotherapy that are being used in cancer therapy. These are monoclonal antibodies, immune checkpoint inhibitors, cancer vaccines and immune system modulators.
A) Monoclonal antibodies (mAbs): These are man-made antibodies made to specifically attack a particular area of the cancer cell. Antigens specific to cancer cells are recognized and copies of the antibodies produced against these antigens are synthesized in the laboratory. These are known as monoclonal antibodies.
Types of monoclonal antibodies that can be used in the treatment of cancer include the following:
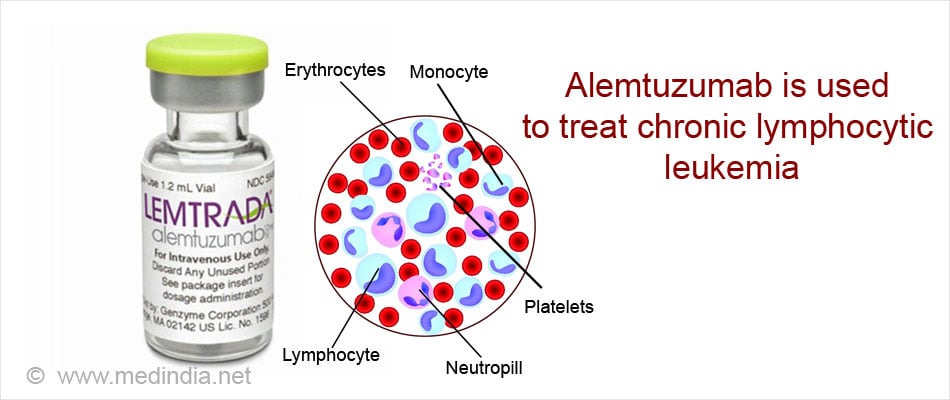
1. Naked monoclonal antibodies are used alone and without any added elements.
- When they attach themselves on a particular antigen, they mark that antigen and attract the immune cells that then start to attack the antigen, e.g. Alemtuzumab used against chronic lymphocytic leukemia (CLL).
- Some antibodies attach themselves to antigens on cancer cells that promote other cancer cells to grow. Thus by blocking the antigen, there is a reduction of cancerous growth. E.g. Trastuzumab attaches itself to the HER2 protein which promotes the growth of breast and stomach cancer cells.
2. Conjugated monoclonal antibodies are tagged along with either certain chemotherapy drugs or a radioactive element that acts as a toxin to cells. The conjugated mAbs circulate in the body till their specific antigen is found. The toxin attached to the antibody is then delivered, and specifically attacks the cancer cells without affecting normal cells.
- An example of radiolabeled mAb is ibritumomab tiuxetan that attaches itself to the CD20 antigen on B lymphocytes and is used to treat non-Hodgkin lymphoma.
- Examples of chemolabeled mAbs include brentuximab vedotin, which is an antibody that is attached to a drug and is used to treat Hodgkin lymphoma and anaplastic large cell lymphoma, and ado-trastuzumab emtansine that is attached to a drug to treat breast cancer.
3. Bi-specific mAbs attach themselves to 2 different proteins, one present on the cancer cells and the other on the immune cells thus bringing them together. E.g. Blinatumomab which is used to treat some types of acute lymphocytic lymphoma, a type of blood cancer.
The side effects of mAbs include allergic reaction, fever with chills, fatigue, nausea and vomiting, headache, diarrhea, decreased blood pressure and rashes.
B) Immune checkpoint inhibitors: When the immune system’s attack is very intense, it could attack normal cells along with abnormal cells. To limit the strength and duration of the immune response, there are certain proteins called immune checkpoint proteins that act as “off” switches and control the system. Cancer cells can engineer these cells up to a point of even suppressing the immune system.
To overcome the effect of cancer cells, immune checkpoint inhibitors can be used. These drugs inhibit the immune checkpoint proteins so as to enhance the immune system. Examples include:
- PD-1 or PD-L1 inhibitors: Proteins called PD-1 are present on immune cells. When PD-1 proteins attach themselves to PD-L1 proteins on normal or cancer cells, they tell the immune cells not to attack those cells. When cancer cells have a lot of PD-L1, there are more bound PD-1 and this protects the cancer cells. Inhibitors of PD-1 and PD-L1 proteins will reverse this effect and make the immune cells attack the cancer cells.
Pembrolizumab and nivolumab that attach to PD-1 are used to treat cancers like melanoma of the skin, non-small cell lung cancer, kidney cancer and Hodgkin lymphoma. Atezolizumab that attaches to PD-L1 is used to treat bladder cancer and non-small cell lung cancer.
- CTLA-4 is another protein present on immune cells that acts as an “off” switch. Ipilimumab is the antibody that attaches to it. It is to treat melanoma of the skin.
C) Cancer vaccines are mostly preventive in nature. Some cancers are caused by certain viruses. For example chronic infection with the Hepatitis B (HepB) virus increases the risk of liver cancer. The human papilloma virus (HPV) has been linked to cervical, anal and throat cancers. Vaccination against the HepB virus and HPV protects individuals from developing the respective cancers.
Cancer vaccines are being developed to treat cancers that are already present. The vaccines either alone or along with other added substances or cells further enhance the immune system against the cancer cells. A vaccine has been approved in the United States to treat advanced prostate cancer that no longer responds to hormonal treatment.
D) Immune System Modulators: These substances do not target the cancer cells directly but stimulate the immune system in a general way. Two kinds of cytokines called interferons and interleukins are examples.
- Interferons (IFN) cause anti-viral responses. They activate white blood cells like killer cells and dendritic cells. So far interferon alpha has been approved and shown to be clinically effective for hairy-cell leukemia, follicular lymphoma, chronic myeloid leukemia and melanoma. Side effects of IFN alpha are flu-like symptoms including chills, headaches, nausea, vomiting and loss of appetite, skin rashes, low white blood cell counts and hair loss.
- Interleukins promote effector and regulatory T cells. Interleukin-2 is being used to treat malignant melanoma and kidney cancer.
The BCG vaccine, which is normally used to prevent tuberculosis, can be instilled into the bladder for the treatment of bladder cancer.
What is New in Cancer Immunotherapy Research?
A) Cell-based therapy - Adoptive Cell Transfer: A new intervention in the field of immunotherapy is to use specific cells of the immune system that have infiltrated into the tumor cells and can thus recognize them. These treatments are still being evaluated in clinical trials.
- T cells that have got into tumor cells are called tumor-infiltrating lymphocytes or TILs. They are extracted from the tumors, grown in laboratories and further activated using cytokines, following which they are infused into the bloodstream again. They have a good recognition for tumor cells which they find and destroy as they are now enhanced to overcome the cancer cells that were previously dominant.
- T cells obtained from the blood can be genetically modified to express a protein called chimeric antigen receptor, or CAR. The modified T cells are grown in labs and infused back into the patient. The CARs which are modified forms of T cell receptors present on the cell surface of a T cell help these cells to attach to specific proteins on the cancer cells. The bound T cells get activated and destroy the cancer cells.
B) Oncolytic viruses: The properties of viruses that of infecting and killing cells can be put to use by altering the same so they attack only cancer cells. These viruses are called oncolytic viruses. An example is talimogene laherparepvec that is used to treat melanomas of the skin and lymph nodes.
C) Newer Vaccines are being made that are used in treatment rather than prevention. Some vaccines are being made from tumor cells (tumor cell vaccines) taken out of the patient concerned or from another patient. After alteration and injecting back into the concerned patient, they help the body attack similar cells in the body.
Vaccines can also be delivered with the help of vectors which are nothing but altered viruses, bacteria, yeast cells or other structures that no longer cause the disease. Vectors aid by triggering the immune system more as they are made from germs.
A novel approach in vaccine therapy is to make them using the cells from the body’s own immune system.
Dendritic cell vaccines: Dendritic cells are intelligent enough to seek out and break down the cancer cells and then present the tumor antigens to T cells. The T cells then start attacking other cells that have the same antigens.
Dendritic cell vaccines are made by removing immune cells from the patient’s blood who has to get treated. This is called an autologous vaccine. The cells are then exposed to agents like cancer cells, parts of cells, or pure antigens to elicit a response and to grow them. The immune cells are thus changed into dendritic cells. This is a complex and expensive procedure.
The dendritic cells are injected intravenously into the patient for a total of 3 times in 2 week intervals to help other immune system cells to attack the cancer. An example of a dendritic cell vaccine is Sipuleucel-T which is approved for the treatment of advanced prostate cancer that can no longer be helped by hormone therapy. To target prostate cancer cells specifically, they are exposed to a protein called prostatic acid phosphatase (PAP) which produces an immune response against the prostrate cancer cells.

Sipuleucel-T does not cure prostate cancer but has definitely extended the lives of these patients by several months. Side effects of this therapy are fever with chills, fatigue, nausea, joint pain and headache.
D) Novel immune checkpoint inhibitors: Combining the inhibitors of two different targets, like nivolumab, which targets PD-1, and ipilimumab, which targets CTLA-4 to treat melanoma has shown better results than targeting only one checkpoint protein. However, this combination comes with a lot of side effects.